What happens when the healthcare system tries to keep up with a world that won’t sit still? Between aging populations, mental health surges, tech revolutions, and pandemic aftershocks, today’s care needs are changing faster than ever.
What happens when the healthcare system tries to keep up with a world that won’t sit still? Between aging populations, mental health surges, tech revolutions, and pandemic aftershocks, today’s care needs are changing faster than ever.
For health professionals, adapting isn’t just helpful—it’s essential. Let’s look at how those in the field can stay ahead of the curve while still keeping their sanity intact.
Understanding What “Care” Means Today
Gone are the days when healthcare was all about flu shots, broken bones, and the occasional appendix. Today, care is an ever-expanding concept. It’s about mental health, chronic disease management, telehealth, community outreach, and even climate-related illness. From wildfire smoke to social isolation, new threats to well-being pop up like apps in a smartphone update.
What’s more, patients are different too. They’re more informed, often by internet rabbit holes, and they want providers who can engage with them, not just treat symptoms. Health professionals must be listeners, educators, tech navigators, and sometimes, reluctant therapists. The role is growing, and so must the preparation.
Investing in Education That Moves With the Times
Training isn’t a one-and-done event. Nurses, doctors, therapists, and allied professionals are expected to evolve with science, policy, and technology. That means going back to school—or at least logging in. Today, healthcare education has finally caught up with flexibility.
For example, Rockhurst online nursing degrees offer options that blend academic rigor with real-world practicality. These programs are designed for working professionals who need to grow without pausing their careers. They also reflect the shifts in care delivery, offering coursework in leadership, community health, and data-informed decision-making.
More importantly, continuing education helps professionals understand the full context of care. For example, how do social determinants like housing insecurity or language barriers affect diagnosis and recovery? Education that prioritizes these questions helps create providers who aren’t just reactive—they’re proactive.
Bracing for the Rise in Chronic Conditions
Chronic illness isn’t just rising—it’s dominating. According to the CDC, six in ten Americans live with at least one chronic disease. These aren’t quick-fix conditions. Managing diabetes, hypertension, COPD, or mental health disorders requires long-term engagement and a multidisciplinary approach.
Health professionals need to build endurance for this kind of work. It means collaborating with nutritionists, social workers, mental health providers, and pharmacists, often all at once. It also calls for better patient tracking, clear communication strategies, and a realistic understanding of what “compliance” means for people juggling jobs, kids, and bills.
Adaptable care plans, tech-based monitoring tools, and cultural sensitivity are no longer nice-to-haves—they’re essential.
Embracing Tech Without Letting It Take Over
Let’s be honest. Some health professionals still treat the electronic health record like a necessary evil. But digital tools aren’t going anywhere. Whether it’s telemedicine, wearable health trackers, or predictive analytics, tech is now woven into every layer of care.
That doesn’t mean providers need to become IT experts. But it does mean understanding how these tools improve efficiency and patient outcomes. Telehealth, for example, isn’t just a pandemic trend—it’s become a lifeline for rural patients, those with limited mobility, and anyone who prefers pajamas to waiting rooms.
Still, there’s a risk. Tech must support human care, not replace it. Providers should prioritize platforms that enhance their workflow rather than complicate it. Learning how to spot the difference is a skill in itself.
Building Mental Resilience (Because Burnout is Real)
Burnout used to be whispered about in hospital break rooms. Now it’s headline news. A 2023 report by the American Medical Association showed alarming rates of emotional exhaustion among healthcare workers. Staffing shortages, moral injury, and relentless patient loads have pushed professionals to the brink.
So, how do you prepare for evolving care needs without losing yourself in the process? Start by treating mental resilience as a skill, not a character trait. That means building routines that include rest, boundaries, peer support, and maybe even therapy.
Organizations, for their part, must do more than offer a pizza party after a tough week. They need to invest in systems that support mental health long term—flexible scheduling, safe staffing ratios, and spaces to process trauma. If we want sustainable care, we need sustainable caregivers.
Getting Comfortable with Community-Based Care
The hospital is no longer the center of the healthcare universe. Increasingly, care happens in schools, homes, shelters, and even barbershops. This shift recognizes that health doesn’t exist in a vacuum—it’s tied to relationships, environments, and resources.
Health professionals should expect to meet patients where they are, sometimes literally. That may include home visits, mobile clinics, or health education sessions in nontraditional spaces. It may also involve forming partnerships with local organizations that know the community best.
This doesn’t mean lowering clinical standards. It means delivering care in ways that are accessible, respectful, and realistic. The more we bring healthcare into everyday life, the less intimidating and more effective it becomes.
Planning for the Unplannable
If COVID taught us anything, it’s that “normal” is fragile. Whether it’s a new virus, a climate event, or a political shift that redefines funding, health professionals need to be ready for curveballs.
This isn’t about fear. It’s about agility. It’s about having protocols, but also having plans B through Z. It means knowing how to triage under pressure, how to communicate when information changes by the hour, and how to support patients who are scared, skeptical, or just plain tired.
The best preparation is a mix of skill, self-awareness, and the ability to learn in real time. That applies to individuals—and the systems they work within.
Adapting to evolving care needs doesn’t mean chasing every trend or working yourself into the ground. It means staying informed, staying flexible, and remembering why you entered this field in the first place. Patients need care that fits a complex, unpredictable world. The professionals who thrive will be the ones who see that change not as chaos, but as an invitation to lead.
P.S. Before you zip off to your next Internet pit stop, check out these 2 game changers below - that could dramatically upscale your life.
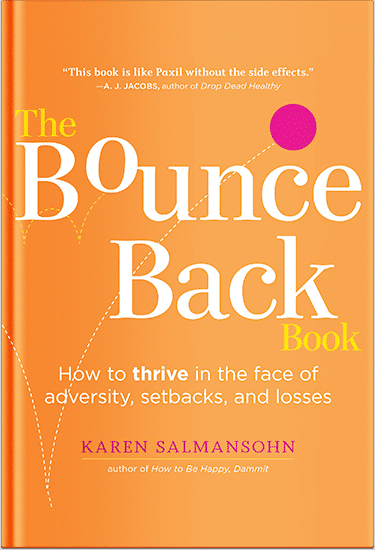
1. Check Out My Book On Enjoying A Well-Lived Life: It’s called "Your To Die For Life: How to Maximize Joy and Minimize Regret Before Your Time Runs Out." Think of it as your life’s manual to cranking up the volume on joy, meaning, and connection. Learn more here.
2. Life Review Therapy - What if you could get a clear picture of where you are versus where you want to be, and find out exactly why you’re not there yet? That’s what Life Review Therapy is all about.. If you’re serious about transforming your life, let’s talk. Learn more HERE.
Think happier. Think calmer.
Think about subscribing for free weekly tools here.
No SPAM, ever! Read the Privacy Policy for more information.
One last step!
Please go to your inbox and click the confirmation link we just emailed you so you can start to get your free weekly NotSalmon Happiness Tools! Plus, you’ll immediately receive a chunklette of Karen’s bestselling Bounce Back Book!


 What happens when the healthcare system tries to keep up with a world that won’t sit still? Between aging populations, mental health surges, tech revolutions, and pandemic aftershocks, today’s care needs are changing faster than ever.
What happens when the healthcare system tries to keep up with a world that won’t sit still? Between aging populations, mental health surges, tech revolutions, and pandemic aftershocks, today’s care needs are changing faster than ever.